by Dr. Mary Ann LoFrumento
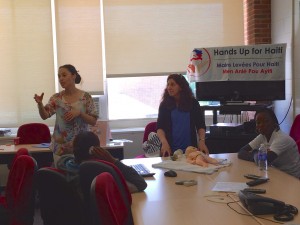
Summertime provided a unique opportunity for Hands Up for Haiti this July. Unlike so many of our missions that are focused on patient care in our various clinics, this particular trip emphasized the investigation of public health issues as well as the health education of young people in Haiti. The team was led by Dr. Jill Ratner and myself, both co-founders and leaders in the organization. As HUFH celebrates its fifth anniversary, the leadership of the organization is taking a step back to evaluate our programs and to ensure that we are addressing the major concerns and the critical needs of the Haitian people in the communities we serve.

Families at Shada Clinic
Our goal on this trip was to initiate discussions with locals about their experiences with water, nutrition, sanitation, and general health/safety practices. Data collected from a selection of these discussions (focus groups) will be used to inform the development of our programs in Cap Haitien so that we can continue to contribute in a way that addresses the needs of each specific community.
This is the first of a series of blogs in which we, the volunteers, want to share stories about the July trip and our experiences. We will also report and discuss some initial findings from our research in subsequent blogs.

July 2015 Team
While this trip emphasized public health and program evaluation objectives, we were joined by Mary Joan Murphy, a nurse practitioner with a Master’s in public health, and several other nurses and nursing students from the U.S. and Canada. Our clinical team was able to examine and interview almost all current patients in our malnutrition program (about 200 children). Of course, we were able to also see any seriously ill children who came to the clinics, but our primary objective this week was the longitudinal assessment of the children in our malnutrition program, specifically in order to determine what steps should be taken upon completion of the 8-12 week Medika Mamba treatment.

Nurse Youselene who helps run our Medika Mamba program orients volunteer nurse Gayrleen.

Dr. Jill Works in the clinic in Bod me Limbe
In terms of our public health objectives, we had an experienced epidemiologist, Dr. Lisa Weiss, Ph.D., to help us evaluate our malnutrition program, and a specialist in conservation management, Dr. Jennifer Thomsen, Ph.D., who has a special interest in researching access to clean water in Haiti. Lisa and Jennifer led focus groups at each one of our four clinical sites: Shada, Bod me Limbe, Open Door, and Jolitrou. The focus groups led by Lisa involved the parents from the malnutrition program (10-12 locals in a session). The focus groups led by Jennifer asked community members about their access to clean water and safe cooking tools. Other key leaders that were interviewed in the community were Madame Bwa, a health care worker in Shada, and two concerned pastors in Bas Limbe. The results from these focus groups will be the subject of a later blog.

Jennifer Thomsen leads a focus group on clean water.

Lisa Weiss leads focus group with mothers whose children are in our malnutrition program.
Our team also included certified EMT college students who, together with the nursing students, were in charge of teaching Haitian youth groups at three of our clinical locations. The teaching topics were related to safe sex, the causes and prevention of common cancers, nutritional practices to stay healthy, and CPR/first-aid. Dr. Margaret Keneman, Ph.D., a French and foreign language education scholar at the University of Tennessee, helped supervise the teaching program. The excitement and enthusiasm for the teaching sessions was palpable on both sides of the desk as our young team members shared their prepared talks with youth leaders in Haiti who can now go back and share the information with their communities. In total, our team members taught approximately 60 Haitian teenagers and young adults, each of whom were awarded certificates at the end of the program.

Nursing student Alyssa with translator Sonel, teaching session on cancer prevention
This teaching program and other aspects of the trip seem to have been especially effective thanks to the active involvement of our on-site Haitian team. In particular, we were often able to pair a native Haitian, such as Dr. Dieula Touissaint and Dr. Manol Isaac, with students teaching in each classroom. We were also fortunate to have two Haitian-Americans on the trip, a nurse, Rosenie Ovil, and a nursing student, Gayrleen Blemur, who greatly helped bridge cultural barriers. Wisly Lindor, a nurse practitioner student who lives in Cap Haitien, also worked closely with our team members in the clinic, the classroom, and the field throughout the trip. He is in the first class to be graduating in Haiti.

Youth teaching session led by Dr. Dieula and Nurse Practitioner Wisly.
At the end of the trip, we were joined by Jonathan Lis, a second year medical student from the University of Connecticut. He was in Haiti on a six-week research assignment to interview parents in malnutrition program in Shada and Bahon. He spent one night with us at Open Door, and worked with us in clinic and focus groups the next day.

Medical Student, Jonathan Lis with two of our nursing students. Keagan Tinney and Alyssa Piparo
We often like to think about what we, as volunteers, bring to Haiti: medical care, supplies, information, and training. But we can also understand our contribution by reflecting on our experiences when we get home. At the end of our week-long trip in July, we asked our volunteers to reflect and we also asked them share what they took away from the trip. The next few blogs will share the reflections of our volunteers. Below are reflections from Jill and I.

Co-founders Mary Ann and Jill reflect on the past five years.
Jill is pleased that we were able to design a procedure to evaluate our programs, which fortunately allowed us to oversee all of our sites and meet with almost all our team members, as well as many of our collaborators on one trip. In her words, “Everything we set out to do really happened!” Jill is also very proud of all the young people, the students, who were so excited, enthusiastic, and engaged in the whole experience. She is equally grateful to our public health specialists and epidemiologist who helped us discover vital information that will inform our efforts to improve the health of the people we serve in Haiti.

Dr. Jill with nursing student Rosenie and HUFH nurse Rose.
Both Jill and I agree that this trip was a culmination of the last five years as well as an emotional look back at what HUFH has accomplished. At the same time, we have our eyes wide open to the future. Specifically, we want to know how we can best serve the people of Haiti and how we can work best with our Haitian medical colleagues.

Watching them grow
On a more personal note, the most meaningful moment of this trip was realizing how tall the children have grown at Bod me Limbe. Their beautiful faces were first captured in my photos and videos when I met them five years ago. Today, they still run up to hug and play as soon as we arrive. We say it on our brochures: “for every child a chance to grow…..” But to see it over time, it’s a sense of satisfaction that has to be felt to be truly understood.
Stay tuned for more blog entries!