By Katie Lynn RN. With contributions by Barbara Rome RN, Andrea Feddes, RN, and Kristen Ward RN, editorial assistance by Mary Ann LoFrumento MD.
My name is Katie Lynn and I’m an ICU nurse in Mount Kisco, NY. Working in a resource limited country was something I had wanted to do from the time I was in nursing school. I envisioned myself in a remote village, surrounded by children. In November 2010, I got my chance to do just that with Hands Up for Haiti. Although I have been a part of several missions in the past, this was my first experience leading a team.

After months of intense planning and preparation, and help from two members of the team who had been leaders in the past, I was still anxious that things would fall apart. We were a team of eight nurses and one pediatrician. The focus of the mission was education: childbirth, breastfeeding, infant resuscitation, developmental disabilities, sexual education, and prevention of relationship violence. It was a wide range of topics and every member had to prepare in advance for these sessions.
Right from the beginning I realized the immense responsibility of this role and the stress that goes with it. Having the flights booked was one thing, making sure everyone got on the plane was another story; making plans for our teaching sessions at the various clinics and hospitals seemed straightforward but getting everyone to where they needed to be at the right time was the challenge. Being a team leader meant saying “Ok, it’s time to go”, instead of being the one saying “When are we leaving?” This was a whole new side of being on a mission and a steep learning curve.
I worried for our safety as well, since we would be tackling sexual assault head on and this could put members of our team in danger. Seventy percent of women in Haiti will experience some type of violence in their lifetime and sexual assault is unfortunately too common and often “accepted” as part of a culture. How would we, a group of women, spread the message in Haiti that rape is wrong and it is a crime.

One of the nurses on this mission was Barbara Rome, teaches at CUNY College and is a Sexual Assault Nurse Examiner (SANE) in New York City. She is a specially trained nurse called in to collect evidence from rape victims and provide support. In this roll she’s also done education with teenagers. Barbara shared, “Violence against women is pervasive, takes many forms and is a global issue. My goal during this mission, was to offer my expertise to young girls and women in Haiti. Preparing my presentations on Sexual Assault and Domestic Violence I wanted to let the women of Haiti know that they are not alone, and that there are services and people available to help.” Barbara was equally unsure about how this message would be received by the community and also concerned that the language barrier and use of translators would affect the ability to communicate affectively.

Another important part of our team were four young nurses from Ontario, Canada, Krsiten Ward, Katrina Bates, Andrea Feddes, and Hope Anne Bechard. In June of 2012, they traveled to Haiti with us and were struck by the complacency that seemed to surround the issue of sexual assault. Their energy and my realization that more needed to be done were the impetus to return on a solely educational mission. Three of them had graduated from nursing school a few weeks prior and were eager to return to Haiti, working on what they would teach while at the same time finishing up their studies.
Kristen Ward, one of the nurses said, “When coming home last year, I felt as if we barely accomplished anything. I returned this June with such mixed feelings, but very hopeful that we would accomplish more.” It was the same for the others, who had been so shocked by the stories they heard a year ago and determined to make a difference.
Before we started we all wondered out loud and to ourselves, “Would they listen to what we had to say?” The answer we found is YES, they will listen. But we needed a little help from our Haitian colleagues.

A contact was made with an amazing Haitian woman, Elvire Eugene, the V-day International representative in Haiti. V-Day is a global activist movement to end violence against women and girls. In Haiti, she runs a powerful organization, Association Femmes Soleil d’ Haiti known as AFASDA. Elvire and her colleagues have already begun to address this topic. The mission of AFASDA is: to work with women and help them to make actions for a more equitable society through their active participation. Our team met with Elvire before we began our work and learned how we can be culturally sensitive when teaching this topic. For Barbara Rome, meeting Elvire was the highlight of her week as they compared stories and compared their work in two countries.

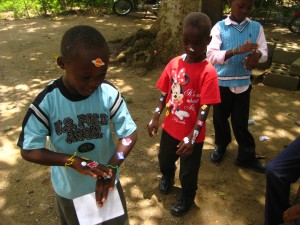
The very next day our team began our work. We were headed to Shada, the slum area of Cap Haitien, where Hands Up for Haiti has been working for the past three years to establish a clinic to serve the mothers and children. The community health worker Madame Bwa arranged for two of our young nurses to address a group of teenagers. They spoke in an outdoor area because the group was so large. It was supposed to be all girls but curious boys appeared and sat around the perimeter . Edia, our translator was a powerful voice to help the nurses talk about puberty, sexual health and then try to approach the topic of sexual assault.

From Andrea Feddes, one of our nurses, “Teaching girls with boys surrounding us was somewhat difficult at times, especially when we got to the section on preventing violence in relationships. We found that when talking about puberty and sex education both the girls and boys were very interested and engaged in conversation with lots of questions. One of the boys even explained to the girls what we had just said and he explained perfectly. But when we began speaking about sexual abuse things got pretty heated. “

“By this point in the discussion there were lots of people around, which included a good mix of men, women, girls and boys. I won’t forget some of the things this one gentleman was saying to us, and our translator. He kept shouting that we weren’t allowed to tell the women that they have rights because they don’t. At one point we were being shouted at and called names. Being in Haiti doesn’t scare me and I’ve never once felt unsafe or uneasy, but with teaching these difficult subjects in a country where women don’t have rights, and are abused, it was a little scary, especially in Shada where education is so limited.”

The nurses got a second chance to teach these topics, this time at Open Door in the more rural area of Bois de Lance. It was market day and the street was filled with young girls. We invited them in for an impromptu class, using older girls to bring younger girls. Suddenly we had a captive audience of girls eager to hear the messages the nurses were teaching. By keeping the group all girls, it was much easier to focus on important topics and give the girls the freedom to ask questions. Everyone breathed easier as the team found a way to educate and empower these young girls.

Meanwhile, Barbara Rome continued her work to educate Haitian nurses on caring for victims of sexual assault. She led the team on a visit to Hospital Fort St-Michel and met with nurses and nursing students about what they might see in a rape victim and how to care for them. Her expertise was evident as she encouraged compassionate care for women that would help them medically and protect them from future violence.
What we found everywhere we went was that women are afraid to report the rape for fear of retribution from the attacker. They also won’t seek treatment for fear they’ll have to report the rape, increasing the risk the woman will become pregnant or contract an STI. In the U.S. women are offered Plan B (where it is legal) and given antibiotics to prevent disease. We hope to help AFASDA develop a program so that women can at least receive treatment without having to report the rape. We also learned that, while domestic violence is illegal in Haiti, the law stops where a marriage begins. Married women have no protection under the law.
Elvire also invited our team to speak at one of her offices near Cap Haitien. About 30 people, mostly teenage girls came and listened, We emphasized that if a man respects you, he won’t put his hands on you and that the girls deserve to be respected. Barbara Rome, “I was amazed at the reception by both the young girls and women. They were attentive, engaged and interested in my presentation”.

One of the most emotional moments of our trip was when of our own translators shared her story with the young women. She spoke of how was beaten and abused for 10 years before she could escape. Afterwards, with our encouragement, the translator exchanged contact information with an AFASDA worker so that her story can help to foster change.
By the end of our week, we were all exhausted, but also very encouraged. Barbara commented, “This trip has made me realize what is needed and how I can help to decrease the incidence of violence. My vision for the future is to help educate the nurses in Cap Haitain on the care of the sexual assault victim, hoping to eventual train nurses to become SANE nurses. “ The young nurses felt that they had accomplished their goal of returning to Haiti with a well organized approach to educating and empowering the young women they met. Perhaps Andrea, our young nurse from Canada, summed it up best, “Nelson Mandela says ‘Education is the most powerful weapon that you can use to change the world.’ This quote speaks volumes to what this trip was all about and what we are trying to do in Shada and the rest of Northern Haiti. My theory is if we can get through to just one person and if that person gets through to others than we have made a difference.”

For me, being the leader of this trip turned out to be a wonderful experience. Like describing a sunset, I cannot fully express how amazing it was to make these connections, to know that we’re doing the right thing, that the women (and some of the men) of Haiti want help to change the culture which is too accepting of relationship violence and sexual assault. It’s enough to keep pushing forward, in hopes that one day rape will be treated in Haiti and the rest of the developing world as the unacceptable crime it is.